Merit Medical Embosphere Microspheres Prefilled Syringe IFU-US User Manual
Page 7
discomfort, and urinary dysfunction. Success was defined as a
moderate or significant improvement for patients who entered
the study with moderate or severe symptoms, and/or no
worsening for patients who entered the study with no or mild
symptoms. Ninety-four of the 107 patients (88%) completed
the bulk symptom questionnaire at 6 months post-treatment.
All 13 patients with missing symptom data at 6 months for any
reason were counted as failures. Table 3 demonstrates that the
majority of UFE patients met the study criteria for success on all
three bulk-related symptoms. This success was generally achieved
by 3 months. Eighty-four percent of the women met the success
criterion for at least one bulk symptom by 6 months.
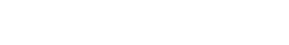
Table 3 - Efficacy: Bulk Symptom Success Rates In Intent-to-
treat Population
Symptoms
6 Months
N/107 (%)
≥ Pelvic Pain
83 (78%)
Pelvic Discomfort
80 (75%
Urinary Dysfunction
75 (71%)
Quality of Life
The SF-12 Health Status questionnaire was used to assess
changes in general physical and mental health status following
treatment. The goal of this endpoint was to demonstrate at
least a moderate improvement in the overall quality of life by the
6-month evaluation. Pre-treatment average scores for the UFE
group were 44.4 ± 8.5 and 45.1 ± 11.9 for the physical and mental
components, respectively, putting this group at slightly better
than the 25th percentile (44.32) of normalized scores published
for the U.S. population of females in general. By 6 months, the
average scores for both the physical and mental questionnaires
had increased significantly to 52.2 ± 6.7 and 52.4 ± 8.8, respectively,
putting the UFE group at the 50th percentile (52.76) of normalized
SF-12 scores (p<0.001 for both measures).
Secondary Efficacy Endpoints
Fibroid and Uterine Volume
UFE patients underwent uterine imaging by MRI or ultrasound
at baseline and follow-up. Uterine and fibroid volumes were
calculated using the formula for the volume of a prolate ellipse
(LxWxDx0.52). Significant decreases in both uterine volume
(measured as including the cervix) and uterine fibroid volume
were recorded for the UFE group by the 3-month evaluation, with
further improvements seen at 6 months (p<0.001 at both time
periods as compared to baseline). Table 4 summarizes the percent
changes in uterine and fibroid volumes at 6 months following
treatment. This table includes uterine volume data from 91 of the
108 UFE Phase II patients (84%) and fibroid volume data from 83
of these patients (77%) who had complete and evaluable imaging
reports at baseline, and at 3 months and 6 months following UFE
treatment. Increases in uterine volumes were reported for 11
patients (12%) and increases in fibroid volumes for 8 patients (8%)
by the 6-month evaluation.
Table 4 - Percent Change in Uterine and Fibroid Volumes From
Baseline
% Decrease at 6 Months
Uterine Volume (cc)
N
mean (SD)
range
91
33.2% (30.5%)
-93.6% to 82.0%
Fibroid Volume
N
mean (SD)
range
83
50.9% (41.7%)
-173.4% to 99.7%
A positive percent change indicates a decrease in volume, while a
negative percent change indicates an increase in volume.
Patient Satisfaction
Both study groups showed a high level of satisfaction with the
outcome of their procedures at both 3 and 6 months. Ninety-two
of 100 UFE patients (92%) and 46 of 47 hysterectomy patients
(98%) who completed the patient satisfaction questionnaire
at 6 months were slightly, moderately or very satisfied with the
outcome of their procedure, with the majority in both groups
being very satisfied.
ADVERSE EVENTS:
Adverse event data is reported for all 132 patients treated by UFE in
both Phases I and II. There were no unanticipated adverse device
effects or unanticipated adverse events reported in this study.
Table 5 presents fifty-one adverse events judged to be probably
or possibly associated with the procedure, which occurred in 37 of
the 132 UFE patients (28%). Seven of the 51 events (14%) occurred
during the UFE procedure, five (10%) between the procedure and
hospital discharge, 17 (33%) from hospital discharge to 1 month
post-procedure, 11 (22%) from 1 to 3 months post-procedure,
4 (8%) from 3 to 6 months post-procedure, and 7 (14%) greater
than 6 months post-procedure. The most common adverse event
was an allergic reaction or rash, which occurred in 8 of the 132
patients (6%), and which were generally judged by the treating
physician to be related to the drugs or contrast agent used
during the procedure. All reactions resolved spontaneously or
with treatment. Four patients had hysterectomies following UFE,
for an overall hysterectomy rate of 3%. One hysterectomy was
performed at 2 months post-UFE due to sustained fever/possible
infection. The other three were elective hysterectomies due to
dissatisfaction with UFE outcome, which occurred at 2, 10, and 11
months post-UFE. One patient (<1%) had a repeat UFE after her
uterine arteries were found to be patent.
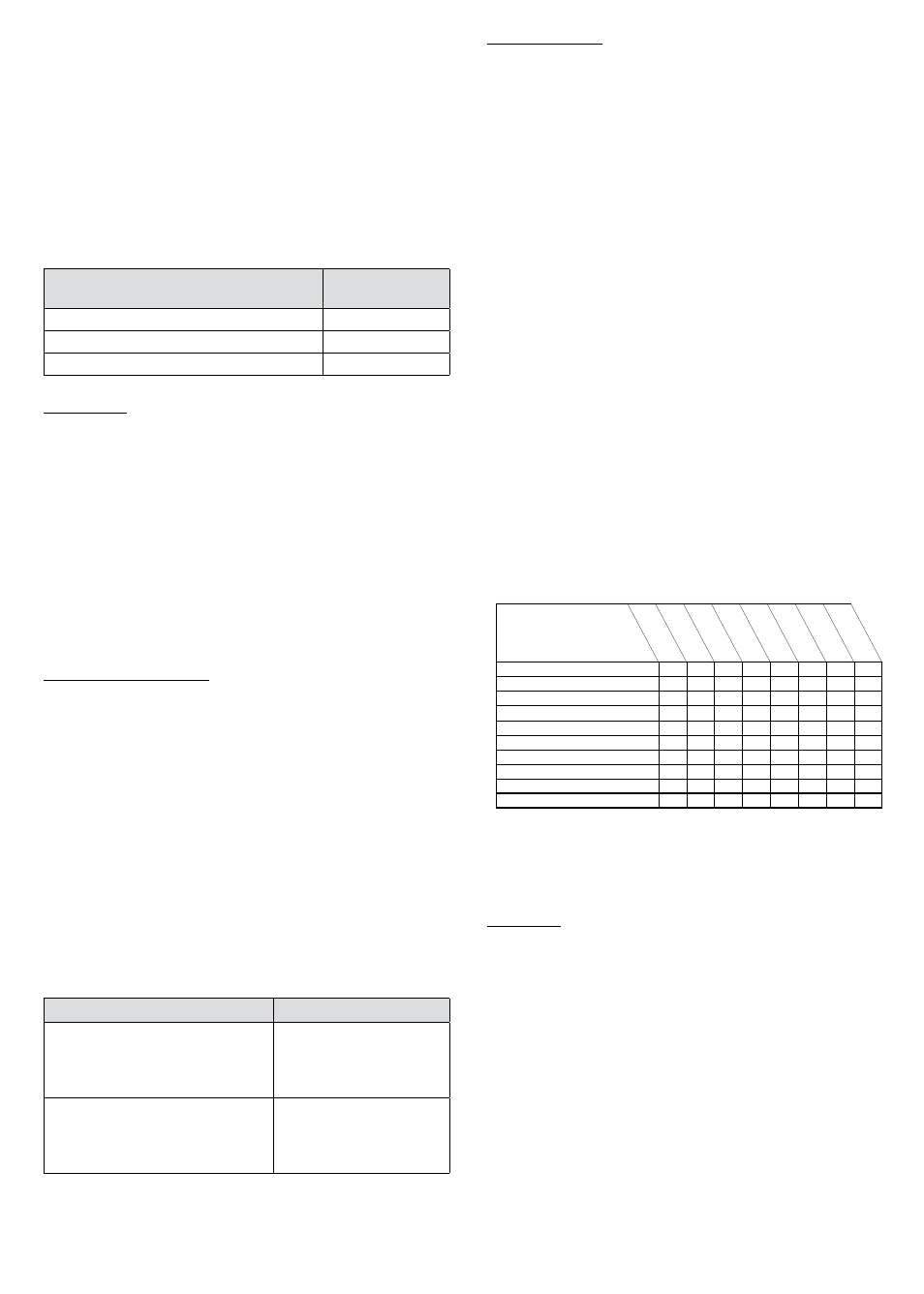
Table 5 - Timing and Type of Probably or Possibly UFE-Related
Adverse events
Time of Event
Event Description
# Patient
Complaints
*
# Events
Pr
ocedur
e
In Hospital
<1 Mont
h
1-3 Month
s
3-6 Mont
h
>6 Months
hysterectomy following UFE
4
4
2
2
Allergic reaction/Rash
8
8
2
3
3
Fibroid/Tissue passage or removal
5
6
2
3
1
Pain related adverse events
4
4
3
1
Catheter/puncture site related injury
6
7
1
2
4
Urinary tract infection/Cystitis
3
4
1
1
1
1
Vaginal Infection/Vaginitis
5
7
2
1
2
2
Vaginal Irritation/Burning/Discharge
2
2
1
1
Other
9
9
4
1
2
1
1
Total
51
7
5
17
11
4
7
*A total of 34 out of 132 patients (26%) experienced one or more
adverse event in this study. The number of patients in this column
reflects the fact that some patients experienced more than one
adverse event.
REFERENCES:
UFE Specific
1. Spies J et al., Initial experience with use of tris-acryl gelatin microspheres
for uterine artery embolization for leiomyomata, J Vasc Interv Radiol, 12:1059-
1063, 2001.
2. Spies J et al., Complications after uterine artery embolization for
leiomyomas. Obstet Gynecol, 100:873-80, 2002.
3. Goldberg J, Pereira L, and Berghella V: Pregnancy After Uterine Artery
Embolization. Obstet Gynecol, 100(5):869-872, 2002.
4. Scialli A: Alternatives to hysterectomy for benign conditions. Int J Fert &
Women’s Med, 43(4): 186-91, 1998.
5. Nikolic B, Spies JB, Campbell L, et al.: Uterine artery embolization: reduced
radiation with refined technique. J Vasc Interv Radiol, 12(1):39-44, Jan 2001.
6. Worthington-Kirsch R, G Popky, F Hutchins: Uterine arterial embolization
for the management of leiomyomas: Quality-of-life assessment and clinical
response. Radiol, 208: 625-629, 1998.
7. Pelage JP, Le Dref O, Soyer P, et al.: Fibroid-related menorrhagia: Treatment
with superselective embolization of the uterine arteries and mid-term
follow-up. Radiology, 215(2):428-431. May 2000.
7