Merit Medical ProGuide Chronic Dialysis Catheter User Manual
Page 2
TROUBLESHOOTING INSUFFICIENT FLOWS
Treatment for insufficient flow will be at the discretion of the physician. Excessive force should
not be used to flush an obstructed lumen. Insufficient blood flow may be caused by an occluded
arterial hole due to clotting or fibrin sheath or because the hole is contacting the vein wall. If
manipulation of the catheter or reversing arterial and venous lines does not help, the physician
may attempt to dissolve the clot with a thrombolytic agent.
MANAGEMENT OF ONE-WAY OBSTRUCTIONS
One-way obstructions exist when a lumen can be flushed easily but blood cannot be aspirated.
This condition is usually caused by tip malposition. One of the following adjustments may resolve
the obstruction:
• Reposition the catheter
• Reposition the patient
• Have the patient cough
• Provided there is no resistance, flush the catheter vigorously with sterile normal saline to
try to move the tip away from the vessel wall.
INFECTION
Catheter related infection is a serious concern of indwelling catheters. Follow institutional
protocol when removing the catheter.
INSERTION TECHNIQUE (2) - COMMON STEPS
PERCUTANEOUS ENTRY INTO RIGHT INTERNAL JUGULAR VEIN
WITH AN OVER-THE-WIRE TECHNIQUE
VENOUS ACCESS AND GUIDE WIRE INSERTION
1. Insert the introducer needle with an attached syringe and advance it into the target vein, in the
direction of blood flow. Aspirate gently as the insertion is made. Aspirate a small amount of
blood to ensure the needle is correctly positioned in the vein.
PRECAUTION: If arterial blood is aspirated, remove the needle and apply immediate pressure to
the site for at least 15 minutes. Ensure that the bleeding has stopped and that no hematoma has
developed before attempting to cannulate the vein again.
NOTE: Mini access (“micropuncture”) is recommended. Follow manufacturers guidelines for
proper insertion technique.
2. When the vein has been entered, remove the syringe leaving the needle in place and place
thumb over the hub of the needle to minimize blood loss and / or air embolism.
3. Insert the distal end of the guide wire into the needle hub (or mini access introducer hub) and
pass it into the vasculature.
4. Advance the guide wire with forward motion until the tip resides in the vena cava.
WARNING: Cardiac arrhythmias may result if the guide wire is allowed to pass into the right atrium.
CAUTION: Do not advance the guide wire or catheter if unusual resistance is encountered.
CAUTION: Do not insert or withdraw the guide wire forcibly from any component. If the guide
wire becomes damaged and must be removed while the needle (or sheath introducer) is
inserted, the guide wire and needle should be removed together.
PRECAUTION: The length of the guide wire inserted is determined by the size of the patient and
the anatomical site used.
5. Remove the needle (or mini access introducer), leaving the guide wire in place. The guide wire
should be held securely during the procedure. The introducer needle must be removed first.
CATHETER PREPARATION AND SUBCUTANEOUS TRACT DILATION
1. The ProGuide catheter is packaged with a guide wire stiffening stylet positioned in the venous
lumen to facilitate placement using the over-the-wire technique.
2. Withdraw the stiffening stylet approximately 2-3 cm and confirm that the stylet tip is not visible
at the end of the catheter.
3. Attach the catheter to the tunneler so that the catheter’s venous lumen at the tip of the catheter
slides over the tri-ball connection and rests adjacent to the sheath stop. This allows the
catheter to be threaded through the tissue as the tunnel is created.
4. Irrigate the arterial lumen and stiffening stylet with heparinized saline and clamp the red arterial
extension prior to catheter insertion.
WARNING: The heparin solution must be aspirated out of both lumens immediately prior to
using the catheter to prevent systemic heparinization of the patient.
WARNING: To minimize the risk of air embolism, keep the catheter clamped at all times when
not in use or when attached to a syringe, IV tubing, or bloodlines.
WARNING: Patients requiring ventilator support are at increased risk of pneumothorax during
subclavian vein cannulation.
CAUTION: Do not clamp the dual lumen portion of the catheter body. Clamp only the clear
extension tubing.
PRECAUTION: Only clamp the catheter with the in-line tubing clamps provided.
5. Determine the catheter exit site on the chest wall, approximately 8-10 cm below the clavicle that
is below and parallel to the venous puncture site.
PRECATUION: A tunnel with a wide, gentle arc lessens the risk of catheter kinking. The distance
of the tunnel should be short enough to keep the bifurcated junction from entering the exit site,
yet long enough to keep the cuff 2-3 cm (minimum) from the skin opening site.
6. Make a small incision at the desired exit site of the tunneled catheter on the chest wall. The
incision should be wide enough to accommodate the cuff, approximately 1 cm.
7. Use blunt dissection to create the subcutaneous tunnel opening at the catheter exit site for
the white tissue ingrowth cuff, midway between the skin exit site and the venous entry site,
approximately 2-3 cm (minimum) from the catheter exit site.
WARNING: Do not over-expand the subcutaneous tissue during tunneling. Over-expansion may
delay or prevent cuff in-growth.
8. Make a second incision above and parallel to the first, at the venous insertion site. Enlarge the
cutaneous site with a scalpel and create a small pocket to accommodate the small remaining
catheter loop (“knuckle”) of the catheter after the peel-away sheath is removed.
9. Attach the tunneler to the catheter’s venous lumen. Slide the tip of the catheter over the
tri-ball connection until it rests adjacent to the sheath stop.
10. Slide the tunneler sheath over the catheter making certain that the sleeve covers the arterial
lumen. This will reduce the drag in the subcutaneous tunnel as the apparitional bump and
arterial port pass through the tissue.
11. With the blunt tunneler, gently lead the catheter and tunneler connection into the exit site and
create a subcutaneous tunnel from the catheter exit site to emerge at the venous entry site.
CAUTION: The tunnel should be made with care to avoid damage to surrounding vessels. Avoid
tunneling through muscle.
CAUTION: Do not pull or tug the catheter tubing. If resistance is encountered, further blunt
dissection may facilitate insertion. The catheter should not be forced through the tunnel.
12. After tunneling the catheter, the tunneler can be removed by sliding the tunneler sheath away
from the catheter and pulling the tunneler from the distal tip of the catheter.
CAUTION: Avoid damage to the catheter by using a slight twisting motion.
CAUTION: To avoid damage to the catheter tip, keep the tunneler straight and do not pull it out
at an angle.
13. Remove the stylet label and tighten down the luer lock nut of the stylet to the blue venous luer
lock connection.
14. Thread the distal tip of the stylet with the catheter over the proximal tip of the guide wire until
the guide wire exits the blue “venous’ luer connection.
15. While maintaining guide wire position in the vein, advance catheter to the desired location. The
distal tip should be positioned at the junction of the superior vena cava and right atrium to
ensure optimal blood flow.
16. PRECAUTION: To help minimize catheter kinking, it may be necessary to advance in small steps
by grasping the catheter close to the sheath.
17. Remove the stylet and guide wire from the venous lumen.
18. Press the catheter small remaining catheter loop (“knuckle”) gently into the subcutaneous
pocket created at the venous entry site.
WARNING: Catheters should be implanted carefully to avoid any sharp or acute angles which
could compromise the flow of blood or occlude the opening of the catheter lumens.
PRECAUTION: For optimal product performance do not insert any portion of the cuff into the vein.
19. Make any adjustments to the catheter insertion depth and tip position under fluoroscopy.
20. Attach syringes to both extensions and open the clamps. Confirm correct placement and catheter
function by aspirating blood from both lumens. Flush each lumen with heparinized saline
(priming volume is printed on the extension tubing clamp). Blood should aspirate easily.
PRECAUTION: If either lumen exhibits excessive resistance to blood aspiration, the catheter may
need to be rotated or repositioned to obtain adequate blood flow.
PRECAUTION: To maintain patency, a heparin lock must be created in both lumens.
PRECAUTION: It is recommended that the venous lumen with the blue luer connection be
oriented cephalad (toward the head).
21. Clamp the extensions immediately after flushing.
22. Remove the syringes and replace with injection caps.
CAUTION: Avoid air embolism by keeping extension tubing clamped at all times when not in use
and by aspirating then irrigating the catheter prior to each use.
22. Correctly position the cuff and tunneled portion of the catheter.
23. Confirm proper tip placement with fluoroscopy. The distal venous tip should be positioned at
the level of the caval atrial junction or into the right atrium to ensure optimal blood flow.
WARNING: Failure to verify catheter placement with fluoroscopy may result in serious trauma or
fatal complications.
SECUREMENT AND DRESSING
1. Suture the pocket created for the small remaining catheter loop (“knuckle”) at the venous entry site.
2. If necessary, suture the catheter exit site.
3. Suture the catheter to the skin with the suture wing.
WARNING: Do not suture through any part of the catheter. If sutures are used to secure the
catheter, make sure they do not occlude or cut the catheter. Catheter tubing may tear when
subjected to excessive force or rough edges.
PRECAUTION: The catheter must be secured / sutured for the entire duration of implantation.
4. Apply transparent site dressing to catheter exit site and the tunneled insertion site using standard
institutional protocol.
WARNING: Do not use sharp instruments near the extension tubing or catheter body.
WARNING: Do not use scissors to remove dressing.
WARNING: Alcohol or alcohol-containing antiseptics may be used to clean the catheter/skin site;
however, care should be taken to avoid prolonged or excessive contact with the solution(s).
WARNING: Acetone and PEG-containing ointments can cause failure of this device and should not
be used with polyurethane catheters.
5. Record the catheter length and catheter lot number on the patient’s chart.
SITE CARE
1. Clean the skin around the catheter.
WARNING: Use of ointments/creams at the wound site is not recommended.
2. Cover the exit site with occlusive dressing and leave extensions, clamps, and caps exposed for
access by dialysis team.
3. Wound dressings must be kept clean and dry.
CAUTION: Patients must not swim or soak the dressing unless instructed by a physician.
PRECAUTION: If profuse perspiration or accidental wetting compromises adhesion of the
dressing, the medical and nursing staff must change the dressing under sterile conditions.
CATHETER REMOVAL
As with all invasive procedures, the physician will assess the anatomical and physiological needs of
the patient to determine the most appropriate catheter removal technique. The white implantable
retention cuff facilitates tissue ingrowth, therefore the catheter must be surgically removed.
WARNING - Only a physician familiar with the appropriate removal techniques should attempt to
remove an implanted chronic dialysis catheter.
CAUTION: Always review institutional protocol, potential complications and their
treatment, warnings and precautions prior to catheter removal.
CAUTION STATEMENTS REGARDING HEMODIALYSIS TREATMENT
• Hemodialysis should be performed under a physician’s instruction using approved institutional
protocol.
• The heparin solution must be removed from each lumen prior to treatment to avoid systemic
heparinization of the patient. Aspiration should be based on institutional protocol.
• Before dialysis begins, all connections to the catheter and extracorporeal circuits should be
examined carefully.
• Accessories and components used in conjunction with this catheter should incorporate
luer-lock adapters.
• Frequent visual inspection should be conducted to detect leaks and to minimize blood loss
or air embolism.
• Repeated over-tightening of blood lines, syringes and caps will reduce connector life and could
lead to potential connector failure.
• If a leak in the catheter tubing or hub occurs, or if a connector separates from any component
during insertion or use, clamp the catheter and take all necessary steps and precautions to
prevent blood loss or air embolism.
• To minimize the risk of air embolism, keep the catheter clamped at all times when not attached
to a syringe, IV tubing, or bloodlines.
• Close all clamps in the center of the extension tubing. Repeated clamping near or on the
luer lock connectors may cause tubing fatigue and possible disconnection.
• Clamping of the tubing repeatedly in the same location may weaken the tubing. Extension tubing
may develop cuts or tears if subjected to excessive pulling or contact with rough edges.
POST DIALYSIS HEPARINIZATION
Follow institutional protocol for heparin concentration. If the catheter is not to be used immediately
for treatment, follow the suggested catheter patency guidelines.
1. Draw the heparin / saline solution into two syringes, corresponding to the amount designated on
the arterial and venous extension tubing clamp. Assure that the syringes are free of air.
2. Attach a syringe containing heparin solution.
3. Open the extension tubing clamp.
4. Aspirate to ensure that no air will be forced into the patient.
5. Inject the heparin solution into each lumen using a quick bolus technique.
PRECAUTION: To maintain patency between treatments, a heparin lock must be created in each
lumen of the catheter.
6. Close extension clamps.
PRECAUTION: Extension clamps should only be open for aspiration, flushing, and dialysis treatment.
7. Remove syringes.
PRECAUTION: In most instances, no further heparin flush will be necessary for 48-72 hours,
provided the lumens have not been aspirated or flushed.
8. Assure luers are capped.
CATHETER PERFORMANCE
PRIMING VOLUMES
• The priming volumes of both the arterial and venous lumens are printed on each extension
tubing clamp.
FLOW RATE
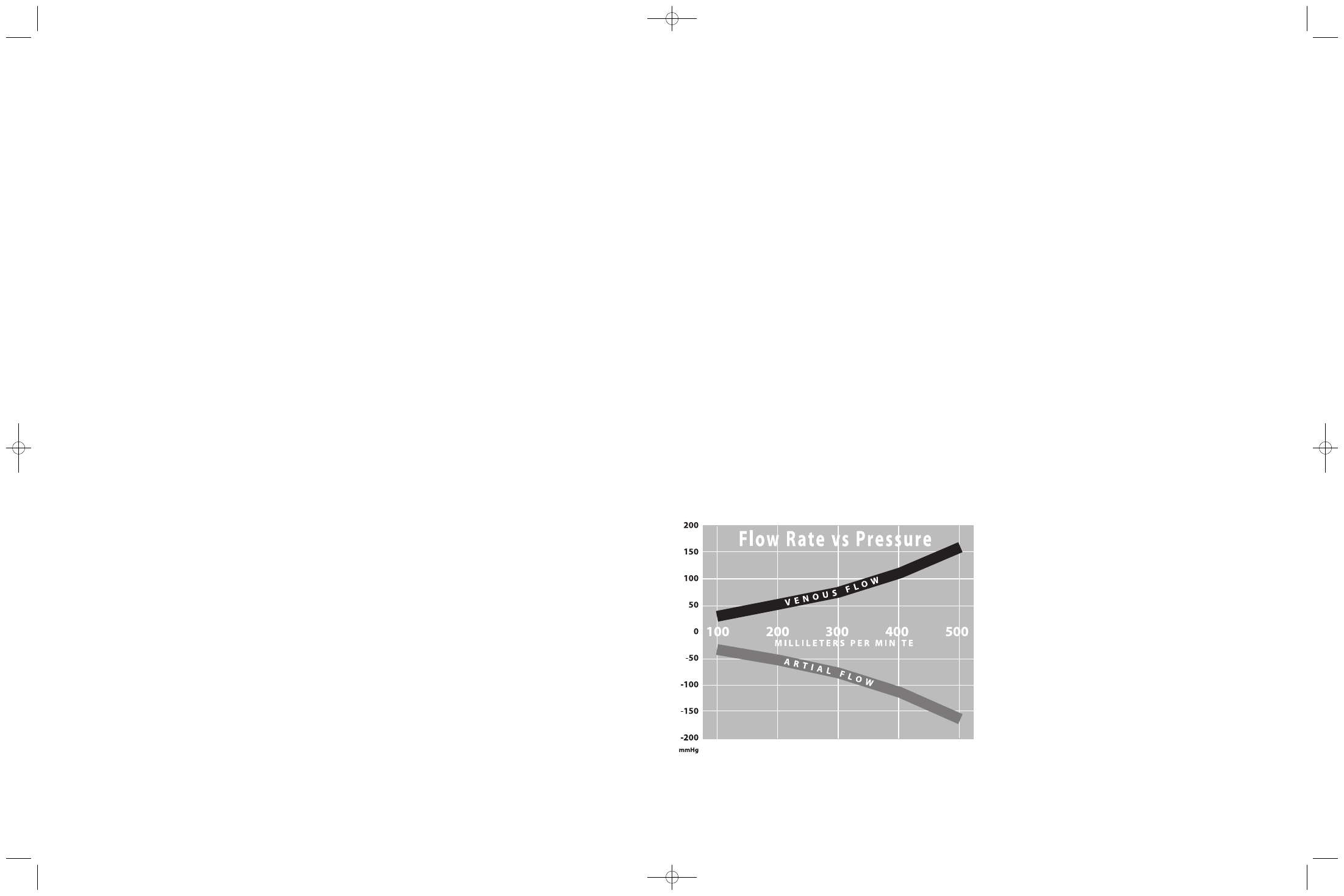
• Typical flow rate vs. pressure with the ProGuide 14.5 FR X 28 cm (tip to hub)
catheter (with side holes)
400863001-A ProGuideIFU 5/15/07 10:05 AM Page 2