Bausch & Lomb Boston Multivision GP Contact Lenses User Manual
Page 3
Burton lamp Application:
1. Replace blue bulbs with ordinary white bulbs.
2. Place Kodak Wratten Filter #47* (blue) over white bulb area.
3. Place Kodak Wratten Filter #12 (yellow) over patient side of viewing lens .
4. Use system in usual manner.
Note: Use of the Wratten filters will also enhance the view of non-UV rigid lenses and corneal fluorescein evalu-
ation.
*Wratten #12 and #47 filters are available from your Authorized BOSTON® Manufacturers in the following kits:
#7503 Slit Lamp Filter kit, #7502 Burton Lamp Modification Kit.
Optimizing Visual Performance:
After an acceptable fluorescein pattern is achie ved, further base cur ve adjustments may still be required to opti -
mized visual performance.
Use the above fitting guidelines to achieve an optimum fit. Place the distance spherical o ver-refraction in a trial
frame and measure the distance and near visual acuities. Use full room illumination at near, and record acuity to
the single letter. If you have excellent distance visual acuity, and less than Jaeger 1 (J1) at near, continue the
trial fitting to optimize near vision.
Fit 0.1-0.2 mm Flatter If:
• The lens does not have enough interaction with the lower lid in down gaze to mo ve the lens upward.
• In down gaze, the lens binds to the superior
cornea, preventing it from maximal translation.
(Lift the upper lid while the patient moves from
primary gaze to down gaze to make this assessment).
• The fluorescein pattern shows significant central
pooling.
Fit 0.1-0.2 mm Steeper If:
• Lid attachment causes the lens to mo ve to an
excessively superior position.
• The lens decenters nasally or temporally
• The fluorescein pattern shows significant central
bearing.
The key to diagnostic fitting is primarily the patient’s visual response. Order the base cur ve that provides the
maximal distance and near vision with an acceptable o verall fit based on fluorescein pattern interpretation.
Initial Lens Power Selection
Step 1:
Perform a spherical refraction o ver the best-fitting trial lens .
Step 2:
If the spherical power of the over-refraction is greater than 4.00D, correct for the ve rt ex distance.
B.
Example:-5.00D at 12 mm = -4.75D at the cornea
+
5.00D at 12 mm =
+
5.37D at the cornea
Step 3:
Combine the spherical over-refraction (corrected for vertex distance if appropriate) with the power of the trial
lens to obtain the final contact lens power ordered.
B.
Example:
Trial lens
-3.00D
Over-refraction (+)+1.00D
_ _ _ _ _ _ _ _ _
Power to order
-2.00D
Initial Lens Center Thickness Selection
For best clinical results, your Authorized BOSTON® Manufacturer will manufacture each BOSTON MultiVision
contact lens with an optimal center thickness . If you choose to specify center thickness, we do not recommend
center thicknesses for minus lenses below the following minimums:
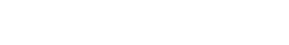
±Spherical
4.00
5.50
7.00
8.50
over-refraction (D)
to
to
to
to
5.25
6.75
8.25
10.00
Corresponding
Power
Compensation (D)
0.25
0.50
0.75
1.00
Vertex Conversion Chart
(12 mm distance)
For minus powers reduce by amount shown.
For plus powers increase by amount shown.
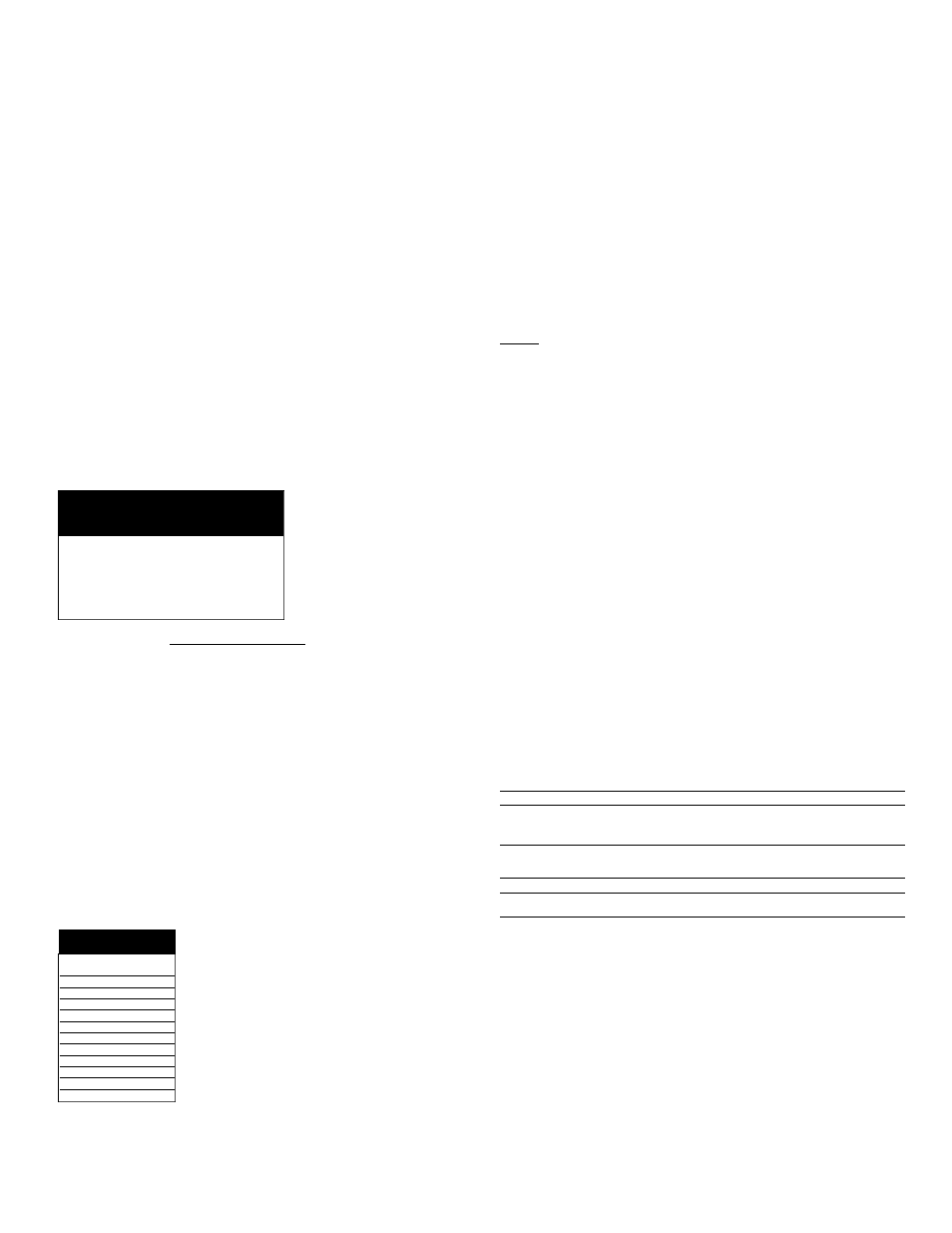
Lens
Recommended
Power
Thickness
Plano
0.24
-0.50
0.20
-1.00
0.18
-1.50
0.17
-2.00
0.16
-3.00
0.15
-4.00
0.14
-5.00
0.13
-6.00
0.12
-7.00
0.11
-8.00
0.10
Minus Lens Minimum
Center Thickness
Remaining Lens Parameter Selection
The final prescription should be provided to the Authorized BOSTON®Manufacturer in a format which includes:
• base cur ve
• center thickness
• diameter of 9.6mm
• distance power
Follow-up Care
Practitioner Note:The BOSTON® MultiVision (enflufoconA) Contact Lenses are not sterile when shipped from
the Authorized BOSTONManufacturer. Prior to dispensing, clean and disinfect the lens(es) according to the
appropriate lens care regimen.
a. Follow-up examinations are necessary to ensure continued successful contact lens
wear. From the day of dispensing, a con ventional follow-up schedule for daily wear should be maintained.
b. Prior to a follow-up examination, the contact lenses should be worn for at least 2 continuous hours and the
patient should be asked to identify any problems which might be occurring related to contact lens wear.
c.With lenses in place on the eyes, evaluate fitting performance to assure that CRITERIAOF
A WELL-FITTED LENS continue to be satisfied.Examine the lenses closely for surface deposition and/or
damage.
d.After the lens removal, conduct a thorough biomicroscopy examination.
1) The presence of vertical corneal striae in the posterior central cornea and/or corneal neovascularization
is indicative of excessive corneal edema.
2) The presence of corneal staining and/or limbal-conjunctival hyperemia can be indicative of an unclean
lens, a reaction to solution preser vatives, excessive lens wear, and/or a poorly fitting lens.
3) Papillary conjunctival changes may be indicative of an unclean and/or damaged lens.
If the CRITERIAOF A WELL-FITTED LENS are not satisfied during any follow-up examination, the patient
should be re-fitted with a more appropriate lens.
WARNING: BOSTON® MultiVision (enflufocon A) Contact Lenses are NOT intended for overnight (extended)
wear.
IN-OFFICE CARE OF TRIAL LENSES
Eyecare practitioners should educate contact lens technicians concerning proper care of trial lenses.
Prior to reusing in a diagnostic procedure or before dispensing to a patient, lenses should be surface cleaned
and disinfected.
RECOMMENDED INITIAL WEARING SCHEDULE
Although many practitioners have developed their own initial wearing schedules, the following sequence is rec-
ommended as a guideline. Patients should be cautioned to carefully follow the wearing schedule recommended
by the eyecare practitioner regardless of how comfortable the lenses feel.
The BOSTON®MultiVision (enflufocon A) Contact Lenses are indicated for daily wear. The maximumsuggested
wearing time for these lenses is:
DAY
WEARINGTIME (Hours)*
1
4 to 8 hours
2
6 to 10 hours
3
8 to 14 hours
4
10 to 15 hours
5
12 to All Waking Hours
6 and after
All Waking Hours
*if the lenses continue to be well-tolerated.
CLINICAL ASSESSMENT
1.Criteria of a Well-Fitted Lens
Patient comfort is largely determined by lens positioning on the cornea.A central or slightly superior, lid-
attachment positioning is generally preferred to enhance comfort and maximize lens performance. Inferior lens
positioning, which interferes with normal blinking and promotes lens binding and 3-9 staining, as well as poor
multifocal visual performance should be avoided.
Ideally, the fluorescein pattern of the lens should demonstrate alignment without excessive peripheral bearing.
Excessive apical pooling or bearing should be avoided.A moderate edge lift is necessary to permit the edge
of the lens to slide over the corneal surface with minimal resistance.
2.Optimizing Fitting Characteristics
In order to achieve optimal performance, it is often necessary to modify the initial trial lens parameters.
Practitioner observations and interpretation of lens positioning, fluorescein patterns, and lens movement are
essential to this process. The following chart summarizes common fitting relationships .
INITIAL TRIAL LENS ASSESSMENT
Optimum
Too Steep
Too Flat
Fluorescein
Parallel to Slight
Excessive Apical Apical Touch
Pattern
Apical Bearing
Pooling
Moderate Edge
Minimum Edge
Excessive Edge
Lift
Lift
Lift
Position
Centered to
Superior
Slightly Superior
Inferior
Excessively
Unstable
Movement
1-2 mm
Less Than 1 mm More Than 2 mm
Comfort
Slight Initial
Initially
Uncomfortable
Sensation
Comfortable
Disposition
Evaluate vision,
Select Flatter
Select Steeper
if optimal,
Base Curve
Base Curve
then Prescribe
3.Problem Solving
Persistent excessive lens awareness:This problem may be due to:the use of incompatible care products;
improper use of care products (i.e., lens cleaning just prior to insertion);three and nine o’clock staining;
deposits on the concave lens surface;accumulation of mucus under the lens;poor edge design, incomplete
blinking or steeply fitted lenses .
Three and nine o’clock staining:If the lens positions low, it should be refit to achie ve a higher position so as to
avoid a false blink pattern.Complete blinking should be encouraged.
Generalized corneal staining:In cases of diffuse staining not apparently related to back surface deposits on
the lens, solution or preser vative incompatibility should be ruled out.
Ocular redness without staining:This problem may be caused by some component of the care solutions such
as preservatives or the presence of pingueculae, infectious or allergic conjunctivitis, or inadequate lens lubri-
cation, including excessive mucus accumulation as occurs in dry eyes.
Excessive development of lens deposits:This unusual problem may be related to:increased mucus produc-
tion, i.e., GPC, keratitis sicca, chronic allergies, etc.The more frequent use of the BOSTON® Rewetting Drops
may be helpful in these cases. In most cases, deposits are easily remo ved by cleaning with original
BOSTON® Cleaner or BOSTON Advance® Cleaner. In the event that deposits cannot be removed by cleaning
the lens should be replaced.