Limitations, Why monitor spv/dpp, Threshold value suggested in the literature – GE Healthcare Arterial Pressure Variation Quick Guide User Manual
Page 3
Arterial blood pressure variation in
GE patient monitoring
Systolic pressure variation (SPV) and pulse pressure
variation (dPP) reflect respiratory changes in arterial
pressure during positive pressure ventilation.
(1, 2, 3)
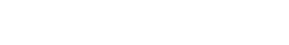
SPV and dPP are calculated from the invasive arterial
blood pressure using the following equations:
SPV [mmHg]= SBPmax - SBPmin
dPP [%]= (PPmax - PPmin) / [(PPmax + PPmin) / 2] * 100
SBPmax and SBPmin represent the maximum and
minimum values of a systolic blood pressure over the
measurement period, respectively.
Values of SPV are represented in mmHg whereas dPP is a
percentage. Both numbers are computed once every five
seconds. The measurement is continuous and trended in
the GE patient monitor. When the monitoring is started
it requires two respiratory cycles before the values are
shown on the screen.
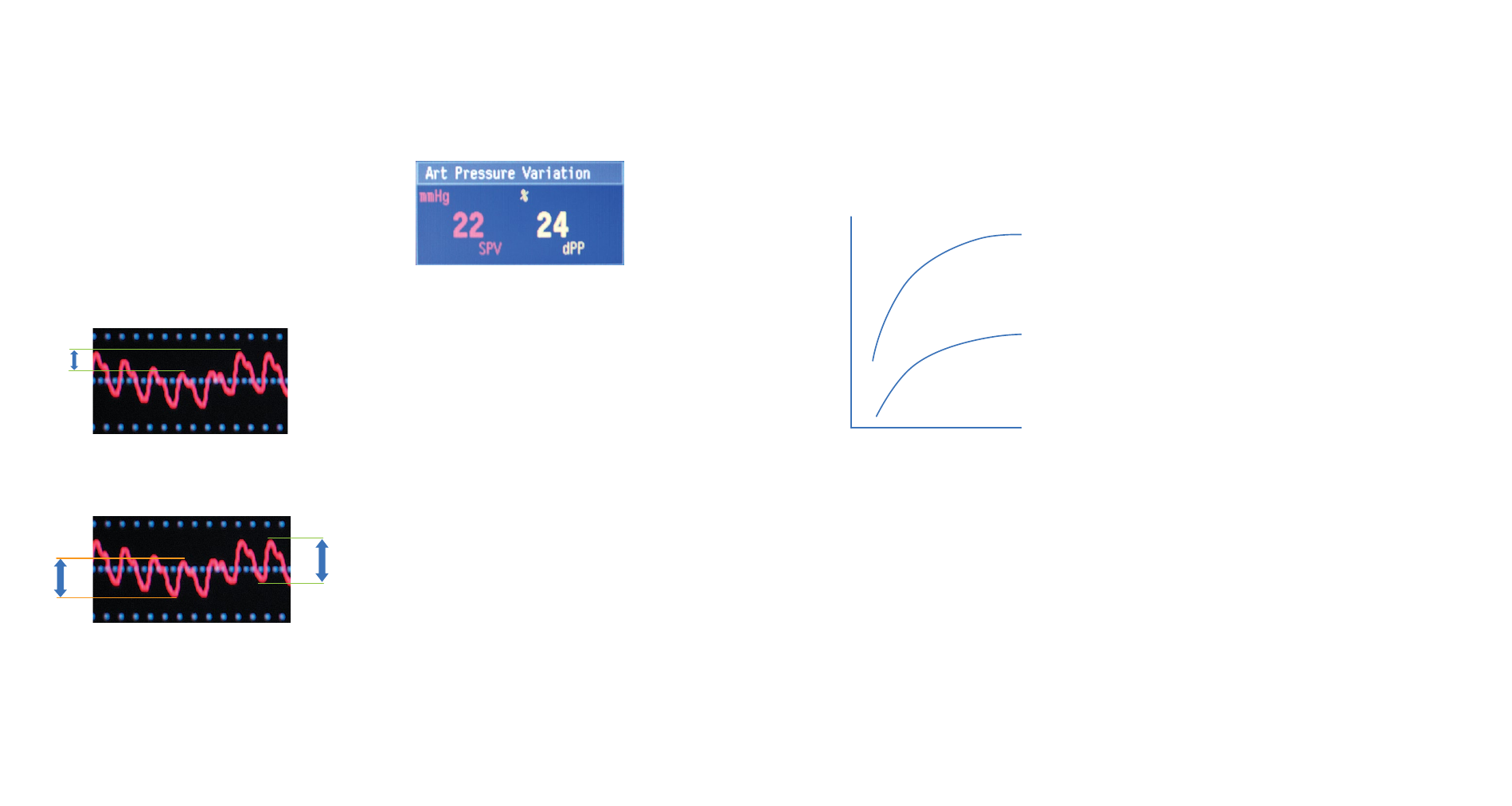
The Frank-Starling curve describes the relation between
stroke volume and preload. The steeply rising section
of the curve represents the area where the patient is
responsive to fluid therapy. It means that a small increase
in preload results in a large increase in stroke volume
and cardiac output. On the other hand, when moving to
the flat area of the curve, the change in preload hardly
makes a difference in stroke volume.
Limitations
There are a few limitations with the clinical use of dPP
and SPV. Firstly, they are only reliable when the patient is
mechanically ventilated.
Secondly, dPP and SPV are reliable only with patients
without cardiac arrhythmias. The algorithm uses the
monitored ECG signal for cardiac arrhythmia recognition.
Since SPV and dPP values are calculated from the
invasive arterial blood pressure waveform, they are
reliable only if the readings of the invasive blood pressure
are reliable. The invasive blood pressure transducer
needs to be at the mid-heart level, adequately zeroed,
and there should not be air in the transducer dome or in
the catheter line.
The GE patient monitor analyzes the invasive arterial
blood pressure signal from which it calculates the arterial
pressure variation parameters. The analysis is done to
the invasive blood pressure channel, which is labeled
“Art” in the patient monitor.
The arterial pressure variation algorithm analyzes the
acquired invasive arterial blood pressure signal and,
therefore, it does not require any further equipment
besides the invasive blood pressure measurement kit.
Why monitor SPV/dPP?
One of the most common questions regarding
hemodynamics has to do with the patient’s fluid
responsiveness: Will the patient’s stroke volume and
cardiac output improve with fluid resuscitation?
In hypovolemic conditions respiratory variations in
stroke volume are higher than normal
1
. However, being
responsive to fluid therapy does not mean that the
patient really needs fluid.
Monitoring arterial pressure variation, i.e. SPV/dPP, helps
to answer the question of fluid responsiveness and can
be used to guide fluid expansion therapy
4
. SPV/dPP
parameters cannot, however, indicate what type of fluid
is the most suitable for the therapy.
SPV
PP
min
PP
max
PPmax and PPmin represent the maximum and minimum
pulse pressures.
Threshold value suggested in the literature
High values of delta pressures indicate responsiveness
to fluid therapy. The values shown in literature for dPP to
indicate fluid responsiveness range from 10 to 15%
(1, 5)
.
If the value is over the limit, it is suggested that the
patient is responsive to fluid loading.
This range holds true when the limitations of the
parameter have been ruled out.
Stroke
volume
Normal heart
Failing heart
Ventricular end-diastolic volume/Preload