Clinical study, Selection of patients, Fitting procedure – Bausch & Lomb PureVision2 for Astigmatism Contact Lenses User Manual
Page 4: Practitioner fitting sets, Wearing schedule, Monovision fitting guidelines, Handling of lens, Care for a sticking (nonmoving) lens, Emergencies, Reporting of adverse reactions
Important Treatment Information for Adverse Reactions
Sight-threatening ocular complications associated with contact lens wear can
develop rapidly, and therefore early recognition and treatment of problems
are critical. Infectious corneal ulceration is one of the most serious potential
complications, and may be ambiguous in its early stage. Signs and symptoms of
infectious corneal ulceration include discomfort, pain, inflammation, purulent
discharge, sensitivity to light, cells and flare, and corneal infiltrates.
Initial symptoms of a minor abrasion and an early infected ulcer are sometimes
similar. Accordingly, such epithelial defect, if not treated properly, may develop
into an infected ulcer. In order to prevent serious progression of these conditions,
a patient presenting symptoms of abrasions or early ulcers should be evaluated as
a potential medical emergency, treated accordingly, and be referred to a corneal
specialist when appropriate. Standard therapy for corneal abrasions such as eye
patching or the use of steroids or steroid/antibiotic combinations may exacerbate
the condition. If the patient is wearing a contact lens on the affected eye when
examined, the lens should be removed immediately and the lens and lens care
products retained for analysis and culturing.
clINIcAl STudy
The following clinical results are provided for informational purposes. It is important
to note that the results below are from a study conducted with the Bausch + Lomb
PureVision
®
(balafilcon A) Visibility Tinted Contact Lens which has the same
lens material, but different lens design (spherical) . The study was conducted with
subjects not requiring astigmatic correction.
STUDY DESCRIPTION
Study Design
The objective of this 12-month study was to evaluate the safety and efficacy of the
PureVision Contact Lenses worn on a 30-day continuous wear basis, compared
to a conventional Control lens worn on a 7-day continuous wear basis. A total of
1640 eyes (820 subjects) were enrolled into this study. Subjects were fitted with
a PureVision Contact Lens on one eye while the contralateral eye was fitted with
a Control lens. Subjects were instructed to replace the PureVision Contact Lens
with a new lens every 30 days, and to wear the Control lens overnight for up to
six consecutive nights per week. Eyes had one night without lens wear after the
scheduled removal. The Control lens was to be replaced with a new lens every 14
days.
Six hundred ten (610) subjects completed the one-year study. Ten subjects
discontinued in the daily wear adaptation period, 182 subjects discontinued during
the extended wear phase and 18 subjects were not dispensed lenses.
Patient Assessments
Subjects were evaluated at follow-up visits scheduled after 24 hours, 10 days, 1
month, 3 months, 6 months, 9 months, and 12 months of lens wear.
Demographics
Subject recruitment was open to adapted and unadapted contact lens wearers.
There were no restrictions as to the subject’s gender or occupation, but subjects
were required to be of legal age (typically 18 or 21) and have the legal capacity
to volunteer. The ages of the subjects ranged from 18 to 74 years of age, with a
mean age of 33.6, and included 574 females and 228 males, with a ratio of 2.52
females to every male. For the PureVision
®
Contact Lens the power range used was
–0.50D to –9.00D. For the Control lens the power range was –0.50D to –8.50D.
The previous lens wearing experience of the subjects that participated in the study
was 5% no lens wear, 43% daily wear, and 51% continuous wear. The refractive
errors of the subjects ranged from –0.25D to –11.75D, and included up to –2.00D
of astigmatism.
SUMMARY OF DATA ANALYSES
Summary of Data Analyses
The key endpoints for this study were:
1. Grade 2 and higher slit lamp findings (safety endpoint),
2. Grade 2 and higher corneal infiltrates (safety endpoint), and
3. Contact lens corrected visual acuity worse than 20/40 (efficacy endpoint).
For each key endpoint, the rates (incidents of endpoint/number of eyes)
experienced by eyes in the PureVision Contact Lens and Control lenses were
calculated. The difference in rates between the two lens types was determined
and a 95% confidence interval for the difference was calculated. For each key
endpoint a “clinically significant difference” in the rates was established before the
study started. These “clinically significant differences” were as follows: 10% for total
slit lamp findings
≥Grade 2, 5% for corneal infiltrates ≥ Grade 2, and 5% for the
acuity endpoint. For example, if the true rates of endpoint infiltrates in the subject
population were 9.99% in the PureVision Contact Lens and 5% in the Control lens,
these rates would be considered substantially equivalent (difference <5%).
In order to be successful for a given endpoint, the upper 95% confidence limit for
the difference in the study rates had to be less than the pre-established “clinically
significant difference.” This means that we are 95% confident that the true difference
is within tolerance. The safety and efficacy goals were met for all three key endpoints.
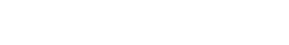
Results are as follows:
PureVision
Control
Relative
Risk/
PureVision
Control
Difference
in %
Upper
95%
Confidence
Level
Clinically
Significant
Difference
Endpoint
n
%
n
%
Slit Lamp
Findings
≥
Grade 2
138
17.5%
139
17.6%
1.0
-0.1%
2.6%
10.0%
Corneal
Infiltrates
≥
Grade 2
23
2.9%
10
1.3%
2.3
1.6%
2.9%
5.0%
Visual
Acuity Worse
than 20/40
0
0.0%
2
0.3%
0.0
-0.3%
0.1%
5.0%
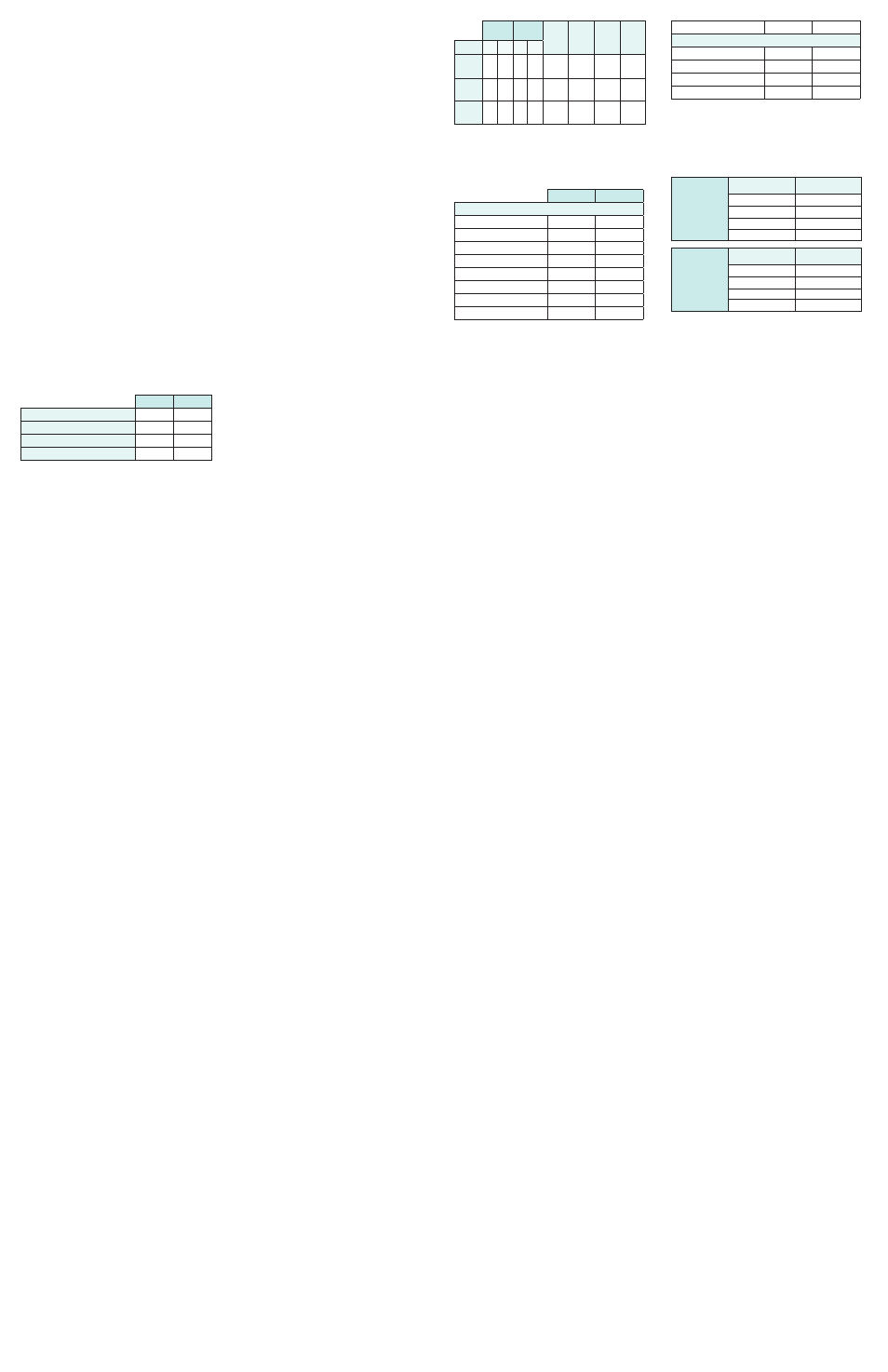
Summary of Slit Lamp Findings
Slit lamp examinations were conducted at every study visit. Each graded slit lamp
parameter was scored on a qualitative grade scale ranging from 0 to 4, with Grade
0 representing the absence of findings, and Grades 1 through 4 representing
successively worse findings. For each study eye, a determination was made for
each parameter as to whether, or not a positive finding was presented at any visit.
The following table describes slit lamp findings
≥
Grade 2 and ungraded slit lamp
findings.
PureVision
Control
Graded Slit Lamp Findings (
≥ Grade2 )
Any Finding
1,2
17.5%
17.6%
Corneal Staining
8.2%
8.4%
Limbal Injection
3.7%
4.3%
Bulbar Injection
5.2%
4.7%
Tarsal Conjunctival Abnormalities
3.9%
3.9%
Corneal Infiltrates
1
2.9%
1.3%
Epithelial Edema
1.3%
1.4%
Epithelial Microcysts
1.0%
1.0%
Corneal Neovascularization
1.0%
1.7%
Ungraded Slit Lamp Findings
Other Anterior Segment Abnormalities
3
13.2%
13.8%
External Adnexa Abnormalities
2.7%
2.7%
Conjunctivitis
2.4%
2.0%
Corneal Striae
0.0%
0.3%
1
Slit Lamp Finding and Corneal Infiltrates
≥ Grade 2 were the safety endpoints for this study.
2
The total of all Graded slit lamp findings does not equal the category of Any Finding.
3
The more common findings identified as Other Anterior Segment Abnormalities included
conjunctival staining; dimple veils; mucin balls; lipid deposits; and ghost vessels.
It should be noted that the PureVision Contact Lens and the Control lens were each
fit on only the right or left eye for each subject. Rates per subject are expected to be
higher when lenses are fit on both eyes.
Corneal Infiltrates
The following table describes the rate of corneal infiltrates according to the lens
power used.
PureVision
Lens Power
Corneal Infiltrates
(
≥ Grade 2)
Plano to – 3.00
1.7 %
– 3.25 to – 6.00
3.2 %
> – 6.00
6.4 %
Total
2.9 %
Control
Lens Power
Corneal Infiltrates
(
≥ Grade 2)
Plano to – 3.00
0.9 %
– 3.25 to – 6.00
1.5 %
> – 6.00
1.3 %
Total
1.3 %
Other Lens-Related Adverse Events
In addition to the outcomes described above, the following lens related adverse
events were noted. This table does not include conjunctivitis or tarsal conjunctival
abnormalities, e.g., giant papillary conjunctivitis.
Other Important Lens-Related Adverse Events
PureVision
Control
Corneal Scar
14 (1.8 %)
5 (0.6 %)
Other Ocular Inflammation*
10 (1.3 %)
2 (0.3 %)
Anterior Chamber Reaction
2 (0.3 %)
1 (0.1 %)
Permanent Loss of Vision
0 (0.0 %)
0 (0.0 %)
*
Other Ocular Inflammation includes episcleritis, scleritis, iritis/uveitis. This condition was
reported in association with other conditions such as keratitis, corneal infiltrates, blepharitis,
corneal abrasion, and contact lens over wear.
It should be noted that the PureVision Contact Lens and Control lenses were each
fit on only the right or left eye for each subject. Rates per subject are expected to be
higher when lenses are fit on both eyes.
Efficacy Outcomes
The contact lens visual acuity was measured at each scheduled and unscheduled
follow-up visit throughout the one-year study. For the 610 subjects that completed
the study, visual acuity of 20/20 or better was reported for 87% and 86% of the
measurements for the PureVision
®
Contact Lens and Control lens, respectively.
Similarly, visual acuity of 20/25 or better was reported 98% and 97% of the times
for the PureVision Contact Lens and Control lens.
Wearing Time
In this U.S. clinical study subjects were required to maintain a minimum wearing
time in order to continue in the study. For the subjects that completed the study, the
average continuous wear time for the PureVision Contact Lens was at least 28.0
days per month, from the 2-Month visit through the 12-Month visit. At these visits the
same subjects reported they were able to wear the PureVision Contact Lens at least
22 days continuously 94% of the times they were asked.
During the course of the study, 15 subjects were discontinued from the study
because they were not able to wear the PureVision Contact Lens for 30 days.
Twenty-one (21) subjects were discontinued from the study because they were not
able to wear the Control lens for 7 days.
Overnight Corneal Swelling
A study was conducted to assess the corneal swelling response induced by
overnight contact lens wear. Twenty-four (24) subjects each wore either a -3.00
–0.75 x 180º PureVision
®
Toric Contact Lens (Test Lens) or a -3.00D PureVision
Contact Lens (Control lens) on the contralateral eye overnight under closed
eye conditions for approximately eight hours. The corneal swelling, measured as
the percent increase in the center thickness of the cornea, of the eyes wearing a
PureVision Toric Lens (4.1%) was compared to the swelling response to the Control
lens (3.6 %). The responses were not statistically different (p-value > 0.20).
SelecTION Of PATIeNTS
The eye care professional should not fit, or provide lenses to, patients who cannot,
or will not, adhere to a recommended care or replacement regimen, or are unable
to place and remove the lenses. Failure to follow handling and cleaning instructions
could lead to serious eye infections which might result in corneal ulcers.
Patient communication is vital because it relates not only to patient selection but also
to ensure compliance. It is also necessary to discuss the information contained in the
Patient Information Booklet with the patient at the time of the initial examination.
Patients selected to wear Bausch + Lomb PureVision
®
2 Toric (balafilcon A) Visibility
Tinted Contact Lenses should be chosen for their motivation to wear contact
lenses, general health and cooperation. The eye care professional must take care
in selecting, examining and instructing contact lens patients. Patient hygiene and
willingness to follow practitioner instructions are essential to their success.
A detailed history is crucial to determining patient needs and expectations. Your
patient should be questioned regarding vocation, desired lens wearing time (full or
part time), and desired lens usage (reading, recreation or hobbies).
Initial evaluation of the trial lens should be preceded by a complete eye examination,
including visual acuity with and without correction at both distance and near,
keratometry and slit lamp examination.
It is normal for the patient to experience mild symptoms such as lens awareness,
variable vision, occasional tearing (watery eyes) and slight redness during the
adaptation period. Although the adaptation period varies for each individual,
generally within one week these symptoms will disappear. If these symptoms persist,
the patient should be instructed to contact his or her eye care professional.
fITTING PROceduRe
1. Pre-Fitting Examination
A pre-fitting patient history and examination are necessary to:
• Determine whether a patient is a suitable candidate for contact lenses (consider
patient hygiene and mental and physical state),
• Make ocular measurements for initial contact lens parameter selection, and
• Collect and record baseline clinical information to which post-fitting
examination results can be compared.
A pre-fitting examination should include spherocylinder refraction and VA,
keratometry, and biomicroscopic examination.
2. Initial Lens Power Selection
a. Select the initial trial lens from the Toric Diagnostic Lens Set with a power
most similar to the patients’ refractive needs, or order a diagnostic lens to the
prescription which most closely matches that of the patient.
b. Place the lens on the eye and allow the lens to remain on the eye long enough
(10 to 20 minutes) to achieve a state of equilibrium. Small variations in the
tonicity, pH of the lens solutions, and individual tear composition may cause
slight changes in fitting characteristics.
c. Allow any increase in tear flow to subside before evaluating the lens. The time
required will vary with the individual.
3. Initial Lens Evaluation
a. To determine proper lens parameters, observe the lens relationship to the
eye using a slit lamp. The toric diagnostic lens is used to optimize lens fitting
characteristics and determine axis orientation. Lens power is determined by the
spectacle refraction.
• Rotation evaluation: The center guide mark should locate at the inferior
limbus. Once oriented, rotational rocking should be limited to less than 5°.
• Movement: The lens should provide discernible movement with:
— Primary gaze blink
— Upgaze blink
— Upgaze lag
• Centration: The lens should provide full corneal coverage.
b. Determine contact lens power. When the toric diagnostic lens does not have an
equivalent to their spectacle Rx, sphero-cylinder over-refractions will often be
inaccurate and confusing. Therefore it is usually preferable to use the spectacle
RX as the only basis for the contact lens power. The sphere and cylinder power
of the spectacle Rx becomes the sphere and cylinder power of the contact lens.
There are two exceptions:
1. If spectacle cylinder power falls between available contact lens cylinder
powers, prescribe the lesser contact lens cylinder power. The sphere power
can be increased -0.25D to compensate if desired. Of course, this can vary
depending on your interpretation of the patient’s subjective responses.
Example: Spectacle Rx: -2.00 -1.00 X 180
Contact Lens Power Ordered: -2.25 -0.75 X 180
2. When the spectacle lens power in any principal meridian is greater than
4.00D, the spectacle refraction should be vertexed to the corneal plane.
This can affect both the sphere and cylinder powers ordered.
Example: Spectacle Rx: -5.00 -2.75 X 180
Contact Lens Power Ordered: -4.75 -2.25 X 180
c. Determine contact lens axis. Note the orientation of the guide mark relative
to the vertical meridian. Regardless of which eye the lens is on, if the rotation is
clockwise but stable, note the amount of rotation, add it to the refractive cylinder
axis and order the resulting axis. If the rotation has stabilized counterclockwise,
again note the rotation, subtract it from the refractive axis and order the resulting
axis. The guide mark can be used to help you calculate the axis of the desired Rx
lens.
Example:
Spectacle Rx: -2.50 -1.25 X 80
Rotation: 20° clockwise
Final Lens Prescription: -2.50 -1.25 X 100
d. Select patient’s lenses
e. Evaluate orientation of final Rx lenses. The orientation of the prescription should
be the same as that observed for the Fitting Set Lenses. For example, if the
lens rotated clockwise 15° then the final prescription lens should also rotate
clockwise 15˚.
4. Criteria of a Well-Fitted Lens
If the initial lens selection fully covers the cornea, provides discernible movement
after a blink, is comfortable for the patient and provides satisfactory visual
performance, it is a well fitted lens and can be dispensed.
5. Characteristics of a Tight (Steep) Lens
A lens which is much too steep may subjectively and objectively cause distortion
which will vary after a blink. However, if a lens is only marginally steep, the initial
subjective and objective vision and comfort findings may be quite good. A
marginally steep lens may be differentiated from a properly fitted lens by having
the patient gaze upward. A properly fitted lens will tend to slide downward
approximately 0.5mm while a steep lens will remain relatively stable in relationship
to the cornea, particularly with the blink.
With your finger, gently rotate the lens approximately 45˚ to the temporal side. It
should reorient within 5 to 10 blinks back to the same stabilized position.
6. Characteristics of a Loose (Flat) Lens
If the lens is too flat, it will:
• Decenter, especially on post-blink.
• Have a tendency to edge lift inferiorly and sit on the lower lid, rather than
positioning between the sclera and palpebral conjunctiva.
• Have a tendency to be uncomfortable and irritating with fluctuating vision.
• Have a tendency to drop or lag greater than 2.0mm on upgaze post-blink.
7. Follow-up Care
a. Follow-up examinations are necessary to ensure continued successful contact
lens wear. From the day of dispensing, the following schedule is a suggested
guideline for follow up.
• 24 hours
• 10 days
• 1 month
• 3 months
• Every six months thereafter
At the initial follow-up evaluations the eye care professional should again
reassure the patient that any of the previously described adaptive symptoms are
normal, and that the adaptation period should be relatively brief. Depending on
the patient’s prior experience with contact lenses and/or continuous wear, the
eye care professional may consider prescribing a one week period of daily wear
adaptation prior to beginning continuous wear.
b. Prior to a follow-up examination, the contact lenses should be worn for at least
4 continuous hours and the patient should be asked to identify any problems
which might be occurring related to contact lens wear. If the patient is wearing
the lenses for continuous wear, the follow-up examination should be conducted
as early as possible the morning after overnight wear.
c. With lenses in place on the eyes, evaluate fitting performance to assure that
CRITERIA OF A WELL FITTED LENS continue to be satisfied. Examine the
lenses closely for surface deposition and/or damage.
d. After the lens removal, instill sodium fluorescein [unless contraindicated] into
the eyes and conduct a thorough biomicroscopy examination.
1. The presence of vertical corneal striae in the posterior central cornea and/
or corneal neovascularization may be indicative of excessive
corneal edema.
2. The presence of corneal staining and/or limbal-conjunctival hyperemia
can be indicative of an unclean lens, a reaction to solution preservatives,
excessive lens wear, and/or a poorly fitting lens.
3. Papillary conjunctival changes may be indicative of an unclean and/or
damaged lens.
If any of the above observations are judged abnormal, various professional
judgments are necessary to alleviate the problem and restore the eye to
optimal conditions. If the CRITERIA OF A WELL FITTED LENS are not
satisfied during any follow-up examination, the patient should be re-fitted with a
more appropriate lens.
PRAcTITIONeR fITTING SeTS
Lenses must be discarded after a single use and must not be used from patient to
patient.
WeARING ScHedule
The wearing and replacement schedules should be determined by the eye care
professional. Regular checkups, as determined by the eye care professional, are
extremely important.
Daily Wear
There may be a tendency for the daily wear patient to over-wear the lenses initially.
Therefore, the importance of adhering to a proper, initial daily wearing schedule
should be stressed to these patients. The wearing schedule should be determined by
the eye care professional. The wearing schedule chosen by the eye care professional
should be provided to the patient.
Continuous Wear (Greater than 24 hours or while asleep):
The wearing schedule should be determined by the prescribing eye care
professional for each individual patient, based upon a full examination and patient
history as well as the practitioner’s experience and professional judgment. Bausch
+ Lomb recommends beginning continuous wear patients with the recommended
initial daily wear schedule, followed by a period of daily wear, and then gradual
introduction of continuous wear one night at a time, unless individual considerations
indicate otherwise.
The practitioner should examine the patient in the early stages of continuous wear to
determine the corneal response. The lens must be removed, cleaned and disinfected
or disposed of and replaced with a new lens, as determined by the prescribing eye
care professional. (See the factors discussed in the Warnings section.)
Once removed, a lens should remain out of the eye for a period of rest
overnight or longer, as determined by the prescribing eye care professional.
MONOVISION fITTING GuIdelINeS
1. Patient Selection
a. Monovision Needs Assessment
For a good prognosis the patient should have adequately corrected distance
and near visual acuity in each eye. The amblyopic patient or the patient with
significant astigmatism (greater than one [1] diopter) in one eye may not be a
good candidate for monovision with the Bausch + Lomb PureVision®2 Toric
(balafilcon A) Visibility Tinted Contact Lenses.
Occupational and environmental visual demands should be considered.
If the patient requires critical vision (visual acuity and stereopsis) it should
be determined by trial whether this patient can function adequately with
monovision.
Monovision contact lens wear may not be optimal for such activities as:
1. Visually demanding situations such as operating potentially dangerous
machinery or performing other potentially hazardous activities; and
2. Driving automobiles (e.g., driving at night). Patients who cannot pass their
state drivers license requirements with monovision correction should be
advised to not drive with this correction, OR may require that additional
over-correction be prescribed.
b. Patient Education
All patients do not function equally well with monovision correction. Patients
may not perform as well for certain tasks with this correction as they have with
bifocal reading glasses. Each patient should understand that monovision can
create a vision compromise that may reduce visual acuity and depth perception
for distance and near tasks. During the fitting process it is necessary for the
patient to realize the disadvantages as well as the advantages of clear near
vision in straight ahead and upward gaze that monovision contact lenses
provide.
2. Eye Selection
a. Ocular Preference Determination Methods
Generally, the non-dominant eye is corrected for near vision. The following
test for eye dominance can be used.
• Method 1—Determine which eye is the “sighting dominant eye.” Have
the patient point to an object at the far end of the room. Cover one eye. If
the patient is still pointing directly at the object, the eye being used is the
dominant (sighting) eye.
• Method 2—Determine which eye will accept the added power with the
least reduction in vision. Place a trial spectacle near add lens in front of one
eye and then the other while the distance refractive error correction is in
place for both eyes. Determine whether the patient functions best with the
near add lens over the right or left eye.
b. Refractive Error Method
For anisometropic corrections, it is generally best to fit the more hyperopic (less
myopic) eye for distance and the more myopic (less hyperopic) eye
for near.
c. Visual Demands Method
Consider the patient’s occupation during the eye selection process to
determine the critical vision requirements. If a patient’s gaze for near tasks is
usually in one direction correct the eye on that side for near.
Example:
A secretary who places copy to the left side of the desk will usually function best
with the near lens on the left eye.
3. Special Fitting Considerations
Unilateral Lens Correction
There are circumstances where only one contact lens is required. As an example,
an emmetropic patient would only require a near lens while a bilateral myope may
require only a distance lens.
Example:
A presbyopic emmetropic patient who requires a +1.75 diopter add would have a
+1.75 lens on the near eye and the other eye left without a lens.
A presbyopic patient requiring a +1.50 diopter add who is –2.50 diopters myopic
in the right eye and –1.50 diopters myopic in the left eye may have the right eye
corrected for distance and the left uncorrected for near.
4. Near Add Determination
Always prescribe the lens power for the near eye that provides optimal near acuity
at the midpoint of the patient’s habitual reading distance. However, when more than
one power provides optimal reading performance, prescribe the least plus (most
minus) of the powers.
5. Trial Lens Fitting
A trial fitting is performed in the office to allow the patient to experience monovision
correction. Lenses are fit according to the directions in the general fitting guidelines.
Case history and standard clinical evaluation procedure should be used to
determine the prognosis. Determine which eye is to be corrected for distance and
which eye is to be corrected for near. Next determine the near add. With trial lenses
of the proper power in place observe the reaction to this mode of correction.
Immediately after the correct power lenses are in place, walk across the room and
have the patient look at you. Assess the patient’s reaction to distance vision under
these circumstances. Then have the patient look at familiar near objects such as a
watch face or fingernails. Again assess the reaction. As the patient continues to look
around the room at both near and distant objects, observe the reactions. Only after
these vision tasks are completed should the patient be asked to read print. Evaluate
the patient’s reaction to large print (e.g. typewritten copy) at first and then graduate
to newsprint and finally smaller type sizes.
After the patient’s performance under the above conditions are completed, tests
of visual acuity and reading ability under conditions of moderately dim illumination
should be attempted.
An initial unfavorable response in the office, while indicative of a guarded prognosis,
should not immediately rule out a more extensive trial under the usual conditions in
which a patient functions.
6. Adaptation
Visually demanding situations should be avoided during the initial wearing period. A
patient may at first experience some mild blurred vision, dizziness, headaches, and
a feeling of slight imbalance. You should explain the adaptational symptoms to the
patient. These symptoms may last for a brief minute or for several weeks. The longer
these symptoms persist, the poorer the prognosis for successful adaptation.
To help in the adaptation process the patient can be advised to first use the lenses in
a comfortable familiar environment such as in the home.
Some patients feel that automobile driving performance may not be optimal during
the adaptation process. This is particularly true when driving at night. Before driving
a motor vehicle, it may be recommended that the patient be a passenger first to
make sure that their vision is satisfactory for operating an automobile. During the first
several weeks of wear (when adaptation is occurring), it may be advisable for the
patient to only drive during optimal driving conditions. After adaptation and success
with these activities, the patient should be able to drive under other conditions with
caution.
7. Other Suggestions
The success of the monovision technique may be further improved by having your
patient follow the suggestions below.
• Having a third contact lens (distance power) to use when critical distance
viewing is needed.
• Having a third contact lens (near power) to use when critical near viewing
is needed.
• Having supplemental spectacles to wear over the monovision contact lenses
for specific visual tasks may improve the success of monovision correction. This
is particularly applicable for those patients who cannot meet state licensing
requirements with a monovision correction.
• Make use of proper illumination when carrying out visual tasks.
Success in fitting monovision can be improved by the following suggestions.
• Reverse the distance and near eyes if a patient is having trouble adapting.
• Refine the lens powers if there is trouble with adaptation. Accurate lens power is
critical for presbyopic patients.
• Emphasize the benefits of the clear near vision in straight ahead and upward
gaze with monovision.
• The decision to fit a patient with a monovision correction is most
appropriately left to the eye care professional in conjunction with the
patient after carefully considering the patient’s needs.
• All patients should be supplied with a copy of the Bausch + Lomb
PureVision
®
2 Toric (balafilcon A) Visibility Tinted Contact Lens Patient
Information Booklet.
HANdlING Of leNS
Patient Lens Care Directions
When lenses are dispensed, the patient should be provided with appropriate and
adequate instructions and warnings for lens care handling. The eye care professional
should recommend appropriate and adequate procedures and products for each
individual patient in accordance with the particular lens wearing schedule and care
system selected by the professional, the specific instructions for such products and
the particular characteristics of the patient.
frequent / Planned Replacement Wear: For complete information
concerning the care, cleaning and disinfection of contact lenses refer to the Bausch
+ Lomb PureVision
®
2 Toric (balafilcon A) Visibility Tinted Contact Lens Patient
Information Booklet.
disposable Wear: For complete information concerning emergency lens care,
refer to the Bausch + Lomb PureVision
®
2 Toric (balafilcon A) Visibility Tinted
Contact Lens Patient Information Booklet.
cARe fOR A STIcKING
(NONMOVING) leNS
If the lens sticks (stops moving), the patient should be instructed to use a lubricating
or rewetting solution in their eye. The patient should be instructed to not use plain
water, or anything other than the recommended solutions. The patient should be
instructed to contact the eye care professional if the lens does not begin to move
upon blinking after several applications of the solution, and to not attempt to remove
the lens except on the advice of the eye care professional.
eMeRGeNcIeS
If chemicals of any kind (household products, gardening solutions, laboratory
chemicals, etc.) are splashed into your eyes, you should: FLUSH EYES
IMMEDIATELY WITH TAP WATER AND THEN REMOVE LENSES
PROMPTLY. CONTACT YOUR EYE CARE PROFESSIONAL OR VISIT A
HOSPITAL EMERGENCY ROOM WITHOUT DELAY.
RePORTING Of AdVeRSe ReAcTIONS
All serious adverse experiences and adverse reactions observed in patients wearing
Bausch + Lomb PureVision
®
2 Toric (balafilcon A) Visibility Tinted Contact Lenses or
experienced with the lenses should be reported to:
Bausch & Lomb Incorporated
Rochester, New York 14609
Toll free Telephone Number
In the Continental U.S., Alaska, Hawaii
1-800-553-5340
In Canada
1-888-459-5000 (Option 1 - English, Option 2 - French)
HOW SuPPlIed
Each sterile lens is supplied in a plastic blister package containing borate buffered
saline solution. The container is marked with the manufacturing lot number of the
lens, the base curve, sphere power, cylinder power, axis, diameter and expiration
date. Store lenses at room temperature (60°F to 80°F/ 15°C to 25°C).
18
17
16
15
22
26
30
21
25
29
20
24
28
19
23
27